Time to Change – the Whalley Range Mental Wellbeing Group – promote a range of activities to support mental wellbeing and promote positive messages about mental health and reduce stigma and discrimination.
Whalley Range Health and Wellbeing

Whalley Range Mental Wellbeing Group aim to promote a range of activities to support mental wellbeing and promote positive messages about mental health and reduce stigma and discrimination.
Time to Change – every Friday
6:00 p.m. to 8:00 p.m.
JNR8, 82 Cromwell Ave, M16 0BG
Contact: 881 3744 or Carol: 07788855544
Come along to a free, volunteer led, self help mental wellbeing group.
Offering:
- Music, Art
- Pool and table tennis
- Tai Chi
- Food
- Good Company
‘It has been the highlight of my week’
Wellbeing group member
About us….
Time To Change, mental health and well being group.
We are a self help group that has been meeting every Friday from 6-8 at JNR8 youth and community centre on Cromwell Avenue, W/R.
There is a range of activities based on what people share and are interested in, ranging from bike repairs, guitar, singing, Tai chi, , computers, pool, but our prime focus each week is cooking and eating a meal together.
The group is usually about 10 to 15 people, who come when they can and we aim to always be there as a point of contact.
We also carry out occasional trips, e.g a day trip to Southport, theatre visits, Vegetarian Society, cookery courses, and we have been involved in the annual Celebrate festival.
The aim of the group is to provide a social space where people feel comfortable, have fun, make friends, and eat cheap, healthy food.
If you would like to come along, please call Carol first on 07788855544, so we can look out for you.
We are also keen to recruit more people who are happy to shop and lead on the cooking once in a while.
Whalley Range Self Help Wellbeing group
Whalley Range Mental Wellbeing Group aim to promote a range of activities to support mental wellbeing and promote positive messages about mental health and reduce stigma and discrimination
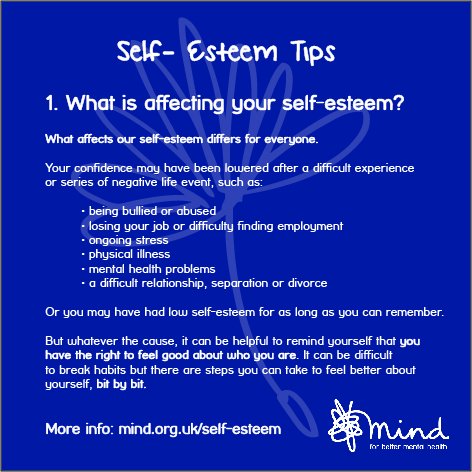
Some of the thoughts/summary of what came out of the initial meeting of the group included:
Challenge stigma
Improve the expertise of staff working with young people in the area in supporting young people with mental health needs
To raise the profile of mental health and wellbeing in a similar way to Age friendly
To promote existing and develop new resources and facilities in the area that support mental wellbeing
Reduce social isolation
Raise awareness of mental health e.g in schools
Improved access to talking therapies
More prevention work with young people
Improve social networks and support for people e.g. Community circles
Improved understanding of the links between physical and mental health
More volunteering opportunities
2. Agreed aims / principles for the group
- To support wellbeing in everything we do
- Confidentiality with regard to group members personal information
- To improve communication
- Not to medicalise people but to take a public health / community approach to mental wellbeing that considers underlying causes
- Reducing stigma and raising awareness of mental health and wellbeing
- Talking about mental wellbeing in a positive way
- Taking a preventative approach
- Being inclusive and representative
- Not making assumptions and looking at evidence
- Building on existing community assets
- Finding sustainable solutions
- Developing partnerships
- Focusing on whats achievable / community response
The group discussed what we understand by mental wellbeing.
feeling good and functioning well feeling in control looking after yourself how you feel when you get up in the morning feeling like yourself
Agreed that the approach should be about improving mental well being for everyone and recognising that mental health will vary across the community and for individuals at different times.
Contact the group for more information on 0161 881 3744
If you’re worried about a child or need advice and support for coping with anything affecting your child’s mental health or wellbeing, there are different ways to seek help.
Online sources of support
Lots of general advice and support can be found online.
For more general advice, see our information on mental health and wellbeing, which includes advice about:
YoungMinds
YoungMinds offers free confidential online and telephone support to anyone worried about the emotional and mental wellbeing of a child or young person up to the age of 25.
- call the free parents’ helpline on 0808 802 5544 from 9.30am to 4pm, Monday to Friday
- email parents@youngminds.org.ukand YoungMinds will respond to your query within 3 working days
The charity also has information for parents and carers about mental health.
MindEd for families
MindEd for families is a branch of MindEd, intended to support parents and those caring for children and young people.
MindEd is an online e-portal offering free, simple advice about children and young people’s mental health for all adults.
Although MindEd is aimed at professionals, parents and carers may also find the information helpful.
Royal College of Psychiatrists
You can also find out more by exploring the Royal College of Psychiatrists’ leaflets for parents and young people.
These include mental health information tailored for young people, parents, teachers and carers.
When to seek professional help
There’s a difference between feeling a bit low from time to time and a serious emotional health problem.
If your child is feeling unhappy and low for a prolonged period of time, or if you have any other serious concerns about your child or young person, it’s time to seek more professional help.
Any professional working with children and young people should know what to do. You may find it helpful to speak to:
- your GP
- someone you trust at school or college – for example, a teacher, pastoral lead, school nurse or special educational needs co-ordinator (SENCO)
- health visitors
- children’s centres
For example, if you approach a teacher about your concerns or to see if they’ve noticed anything, they might speak to different staff working in the school. For example, a school counsellor, a support worker or, in many areas, a mental health support team for schools and colleges.
If the problem is more complex, the professional you initially approached may suggest getting help from colleagues with more specialist training.
A GP might refer a parent of a child with behaviour problems to a local parenting programme, or a young person who’s depressed might be referred to specialist children and young people’s mental health services (CYPMHS).
You should contact your local support services immediately if you’re aware of a child or young person at serious risk of harm.
How do I get help from specialist CYPMHS?
Getting help from a specialist CYPMHS is different depending on where you live. Waiting times can vary too.
Most CYPMHS have their own website, which will have information about access, referrals and more, including phone numbers, so you can get in touch directly for detailed advice.
You can also look at your local clinical commissioning group (CCG) website and search for children and young people’s mental health.
You can also look at your local clinical commissioning group (CCG) website and search for children and young people’s mental health.
There are many services to go to for help without having to ask for a referral, including crisis helplines that anyone can call.
Look up local services that provide mental health support for young people, including phone numbers and website details.
Read about where to get urgent help for mental health.
Read about voluntary community-based youth information services – which often have drop-in sessions for advice and professional help.
Links for Parents/Carers
- Advice for parents and carers talking mental health with young people at secondary school
- Advice for parents and carers talking mental health with young-people at primary school
- Anna Freud parents and carers child in mind series.
- MindEd for Families(parents concerns
- Listen First – resources for parents and carers
- The Anxious Child: A booklet for parents and carers wanting to know more about anxiety in children and young people
- Public Health England’s Every Mind Matters: Every Mind Matters Top tips
- Barnardos: see hear respond support hub
- NSPCC Learning Hub child-mental-health
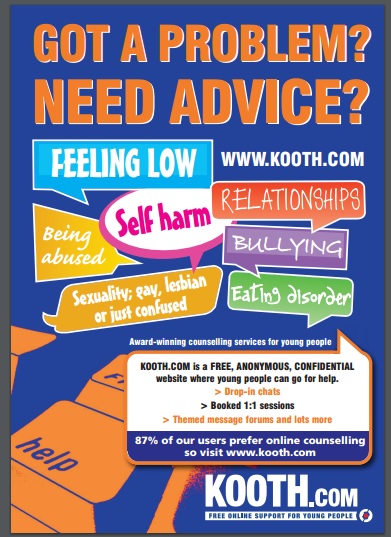
Kooth.com
1 in 5 children and young people suffer from mental health illness in any given year. At Kooth, we believe every young person has the right to thrive and to access high quality mental health care.
Kooth.com is commissioned by the NHS, Local Authorities, charities and businesses to provide anonymous and personalised mental health support for Children and Young People. With over 4000 logins per day, we provide end to end support whatever the need.
Kooth is an online counselling and emotional well-being service for children and young people, available free at the point of access.
Kooth is:
- Safe, confidential, anonymous
- Free at the point of need
- Available through a smart phone, tablet or computer
Kooth helps to reduce wait times for young people seeking help and removes stigma around mental health. Kooth integrates with face-to-face local services to ensure a seamless transition for young people. XenZone’s team of accredited counsellors, therapistsand support workers provide guided, outcome-focused help for each individual.
Kooth works with local authorities, CCGs, mental health trusts, charities and other organisations to provide early intervention support with clear escalation and de-escalation pathways.
We take safeguarding and clinical governance extremely seriously. The safety and well-being of our users is of our upmost priority
Who to contact
Contact Name
Tom Boroughs
Contact Position
Kooth Engagement Lead
Telephone
0753 839 5528
Website
If you are struggling with stress, feelings of anxiety or your mental health
See the NHS mental health and wellbeing advice website for self-assessment, audio guides and tools that you can use. For more information and ways to look after your mental health and wellbeing during the coronavirus (COVID-19) outbreak visit mind.org.uk
Links for Wellness
Tips for looking after your wellbeing from Manchester Mind
Free counselling from Talk Listen Change
Recommended mental health apps
Mental Health Foundation: How to look after your mental health during the Coronavirus outbreak
Greater Sport: Ways to keep moving
https://www.mentalhealth.org.uk/coronavirus
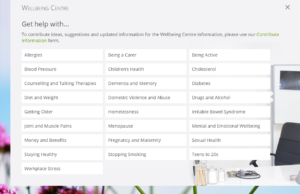
Do you know that most GP surgeries have a useful resource if you visit their website online services – also known as Footfall – and click on the tab that says ‘Wellbeing Centre’?
The Wellbeing centre includes information, links and advice and includes details of local support services. Organisations providing support can contribute ideas to add to the Wellbeing Centre information by completing a form.
FootFall is designed to help patients navigate their way to find help in exactly the way they would if they walked into reception. The home page of FootFall is clearly laid out to help patients manage their health more easily and request advice from a health professional.
The sites are customised by each surgery and look similar to this:
Samaritans: Showing kindness to someone when they’re struggling to cope can make a huge difference. We’ve launched some new guidance to give you the practical tools to support someone who’s having a tough time. bit.ly/2Z6rIRL

Freephone helpline to support most vulnerable in Manchester
A new freephone helpline to support the most vulnerable people in Manchester during the Coronavirus pandemic will go live on from 8.30am from Monday 30 March 2020 and this will sit alongside our comprehensive online portal www.manchester.gov.uk/coronavirus where people can access up to date information immediately.
This new service will initially offer support to:
- People over the age of 70 who are self-isolating and have no support network
- People who have received a letter from the NHS advising they are at higher risk or are medically vulnerable according to government criteria
- Those who are self-isolating with no support networks (ie. friends or family).
Help will also be available, but not limited to, other groups such as carers, care leavers or young carers.
The primary needs that call handlers can help with are:
- Delivery of food
- Delivery of medication
- Combating loneliness
- Managing fuel top-up payments
The Hub’s freephone number is: 0800 234 6123 and lines are open Monday to Saturday, between 8.30am and 5.30pm.
The helpline is being operated by redeployed Manchester City Council staff.
Every Mind Matters has now released expert advice and top tips on how to look after your mental wellbeing if you need to stay at home during the coronavirus (COVID-19) outbreak. It also includes guidance if you’re feeling worried or anxious about the outbreak.
Please visit: www.nhs.uk/oneyou/
Advice if you’re anxious
Looking after mental health and wellbeing during the Coronavirus outbreak
Here are some tips and advice on looking after your mental health and wellbeing during the COVID-19 outbreak, including when staying at home for a prolonged period.
- Get the facts – avoid speculation and only look up information from reputable source such as gov.uk
- Stay connected – At times of stress, we work better with support. Try to keep in touch with your friends and family, or contact a helpline for emotional support.
- Involve children and family – explain the facts, but try to avoid over-exposure to coverage on the virus.
- Try to anticipate distress – It is normal to feel vulnerable and overwhelmed as we read news about the outbreak. It is important to acknowledge these feelings and remind each other to look after our physical and mental health. Try to reassure people you know who may be worried.
- Manage your media intake – There is extensive coverage about the outbreak in the news. It is important to keep informed and educate yourself but if you find watching, reading or listening to the news is causing you distress then you should limit your intake
- Mentalhhealth.org has some more detailed tips
Look after your wellbeing while staying at home
We know that staying at home for a prolonged period of time can be difficult, frustrating and lonely for some people and that you may feel low. It’s important to remember to take care of your mind as well as your body and to get support if and when you need it.
Do things you enjoy
Think about things you can do during your time at home. People who have successfully completed a period of staying at home have kept themselves busy with activities such as cooking, reading, online learning and watching films. If you feel well enough you can take part in light exercise within your home or garden.
Living Life to the Full provides free online courses for Greater Manchester residents covering low mood, stress and resiliency. Work out why you feel as you do, how to tackle problems, build confidence, get going again, feel happier, stay calm, tackle upsetting thinking and more.
Manchester Mind: We need your help – Emergency Food Response
15/05/2020
Good Mood Food meets Food For All
As we mark Mental Health Awareness Week (18-24 May), we are promoting this year’s theme of “kindness” by urging the public to display their own acts of kindness, towards themselves and with one another. Meanwhile we want to highlight our own acts of kindness as a part in the city-wide community food response and ask for your help to enable us to carry out this vital work for people experiencing food poverty.
Good Mood Food, the award-winning outside catering enterprise, has been serving nutritious and vibrant food since 2005. 100% of profits are re-invested into Manchester Mind, enabling us to continue our vital work across the city, in particular supporting people facing food poverty through the Food for All project.
In 2015, Manchester Mind was the first organisation in the city to pioneer weekly Pay What You Can lunch sessions, and we are proud to say that since then our Food for All project has served over 50,000 free or heavily subsidised meals to vulnerable people in our community cafes
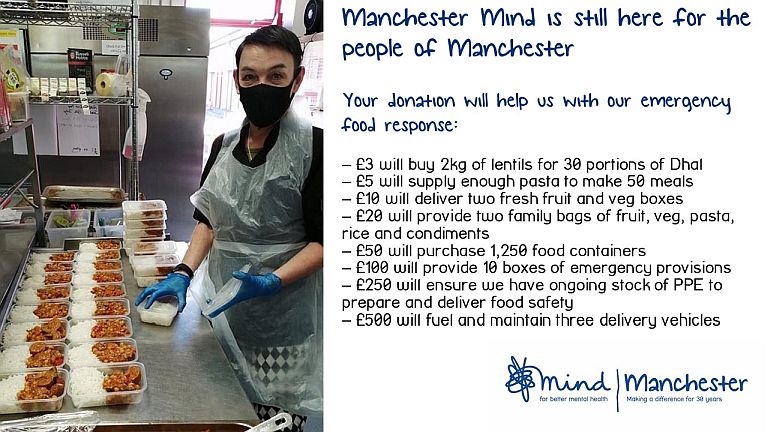
Read more and find out how to support Manchester Mind: https://www.manchestermind.org/manchester-mind-manchester-kind/
Did you know 1 in 20 people might have a personality disorder? Our guide helps you to better understand personality disorders with lots of tips to help! Read, download & print the guide here, along with 12 other guides 

 http://buzzmanchester.co.uk/information/mentalhealthguides…
http://buzzmanchester.co.uk/information/mentalhealthguides… #MentalHealth #BuzzManchester

Find out more: http://www.time-to-change.org.uk/
Mind is inviting people to take part in its third annual Big Mental Health Survey. If you have tried to get support through your GP or a voluntary organisation, Mind want to hear from you.
The survey is open to anyone aged 16 years or older, with personal experience of mental health problems. The information gathered helps better understanding of people experiences of mental health support provided by the voluntary sector and primary care services. It also captures people experiences of discrimination.
You can share your views and experiences by taking part on-line here: http://www.bigmentalhealthsurvey.com/
Social prescribing in practice
GP Dr Mohan Sekeram and link worker Ray Hautot feature in two new videos, which highlight the positive impact their social prescribing service is having on patients. Working with GPs and staff at Wideway Medical Centre, Ray provides tailored support for patients who may benefit from taking part in local activities.
Since introducing social prescribing, the practice has reported fewer GP appointments and attendances at A&E while people health and wellbeing have improved.
The NHS Long Term Plan will see 1,000 social prescribing link workers in place by 2021, with more after that, helping 900,000 more people to benefit from similar schemes.
Sorted. Young People Advice Drop-in.
Events Date: Every Wednesday 2 – 4 pm | Location: Children & Young People Service (CYP), 709 Stockport Road, Levenshulme, M19 3AG

Are you 16-25? Struggling with benefits, work, housing, studies, or money worries? Have things started to affect your mental health?
Come and talk things through with one of our advisers at our weekly drop-in and we can try and help you get things sorted.
We are open every Wednesday from 2-4pm.
Find out more about our Children and Young People Services here

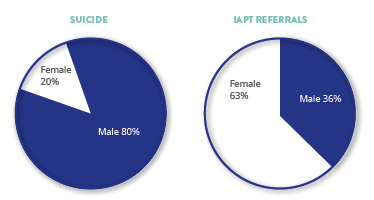
This month has been Men Mental Health Month.
Weve told men stories, shared tips for looking after your mental health, shared the sobering statistics and topics about mental health, shared conversations between men talking about mental health, and invited you to support our work.
Weve been working on that mission to address men specifically for several years now. In 2010 we published Grouchy Old Men – a guide for services coming into contact with men over 50 to consider their mental health needs. Ever since, weve been looking for ways to engage men with the work that we do.
We have created films for Royal Mail Group and Mace Group to enable a largely male workforce to start to talk about mental health.
Through our peer support and self-management we have the opportunity to take the approach into Parc Prison – an all-male environment. 120 prisoners received training on self-management.
We created a fundraising initiative Curry & Chaat specifically to get men involved in community activities.
Men mental health matters all year round! we will continue to bring together research evidence with the perspective of people with lived experience to develop programmes help prevent mental health problems – whether that is growing resilience for all men in the workplace or reaching the most vulnerable men in the country and helping them rebuild their mental health.
Exercise and relaxation for health & Wellbeing
https://soundcloud.com/user-932076252/breathing-space-meditation
Manchester Mind resources: https://www.manchestermind.org/resources/#
GMP and NHS Launch Mental Health Support Service – A brand-new NHS service based within GMP Communications Centre will support the police to respond to mental health-related calls.

Join our yoga classes on Mon (Hulme) or Friday (Harphurhey). Free/donations. All welcome. Call Andrea 07548 023340
Manchester Mental Health Choir
Are you 18 years and over? Are you /have you previously experienced mental health difficulties? Then we invite you to join us in finding fun, friendship and a voice through song.
The Manchester Mental Health Choir will meet every Wednesday during term time. Led by Choir Master Dan McDwyer.
Our aim is to create a safe, fun and non-judgmental environment for you to make new friends, share experiences and join together as one voice. Psychology studies show us choirs have a positive impact on mental wellbeing. The new friendships remind people they are valued and belong. Singing relieves symptoms of anxiety and depression and group singing releases chemicals that make you feel happier. So put your hairbrush down and sing with us at the Bridgewater Hall everyWednesday from 7pm.
Please register your interest through Eventbrite. https://www.eventbrite.co.uk/e/manchester-mental-health-choir-tickets-42984617147?aff=eac2
If you have any questions please email info@triplec.website
All we ask is a contribution of £1 your energy and enthusiasm.
Positive Vibrations Music Project

A new local music project that has been set up by African and Caribbean Mental Health Services for people from all cultures, struggling with mental health problems such as anxiety and depression or learning difficulties and autism.
The project is called “Positive Vibrations” and is based at the Windrush Millennium Centre on Alexandra Road in Units 17 and 18.
We have group sessions throughout the week where people come along to socialise, jam and play songs. Our Tuesday session is at capacity but we have 2 other sessions that currently still have room:
Thursday 10.30am – 4.00pm
Friday 1.00pm – 4.00pm
We are also starting to develop a songwriting session on Wednesdays 2.00pm-4.00pm.
It is also possible to book time on an instrument if someone just wants to have a try or practice.
There are also volunteering opportunities for anyone with at least basic musical and/or mental health experience.
www.facebook.com/
If you would like more information, please don’t hesitate to contact me at this email address or using the details below.
Yours faithfully
Daniel Smith
Music Project Coordinator
African and Caribbean Mental Health Services
Windrush Millennium Centre
70 Alexandra Road
Moss Side
Manchester
M16 7WD
Tel; 0161 226-9562
Fax: 0161 226-7947
www.acmhs-blackmentalhealth.
Creative Conversations
The Creative Conversations group came out of Live Well: Make Art – initially an 8 week pilot project – but so successful that we have continued meeting each week.
This GM led Project aim was to initiate a set of neighbourhood conversations to establish whether or not people living in a specific neighbourhood would be interested in an arts, health and social movements initiative to test how communities, arts and health practitioners can work together to reduce loneliness and social isolation and improve health and care outcomes.
See the film below for details of all of the Greater Manchester projects that were piloted as part of this initiative…
http://mentalhealthmates.co.uk/
Mental wellbeing at work
Three out of five people have experienced mental health issues due to work.
12.5 million working days were lost due to work-related stress, depression or
anxiety in 2016 and 2017.
Tight deadlines, too much responsibility and lack of managerial support are
the main factors causing work-related stress, depression or anxiety.
Samaritans are on a mission to change this. Together, we can create happier,
healthier and more productive workplaces, where employees feel supported and
where no one has to cope alone. Read the full document:
samaritans_witc_bro_a5_2018_web
Stories and experiences of mental health
It's OK to talk about mental health when you are doing something else. You might even find it easier to start a conversation. pic.twitter.com/ZNhezoac9r
— Time to Change (@TimetoChange) April 11, 2018
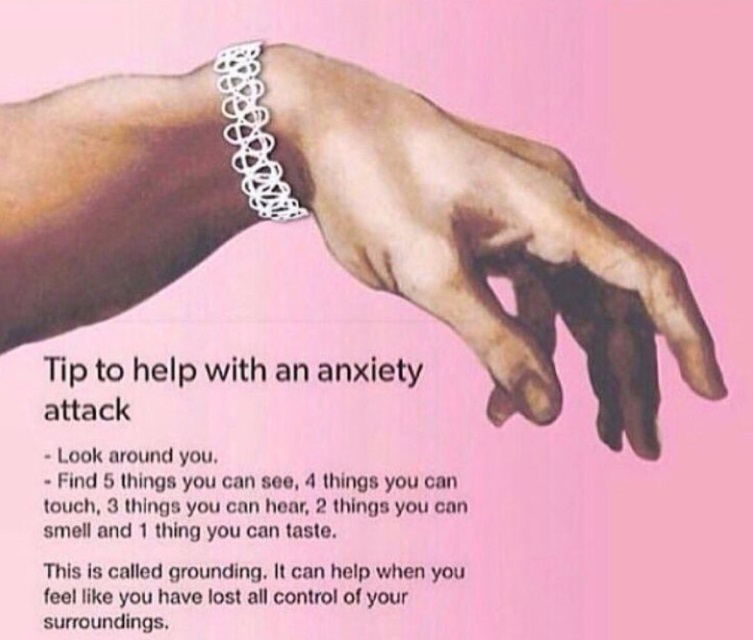
Anxiety Sucks
My anxiety is like a stop button.
Like a warning button.
It tells me when things are scary, when I should worry.
It not like a voice because i can’t hear it. It like a sign.
I can’t always control it, but occasionally it can be negotiated with.
I can reason with it, on good days anyway.
On bad days it doesn’t care.
I will have to deal with a stomach sinking bad feeling, also accompanied by a sick feeling and a feeling of wanting to cry or escape.
It a strong feeling. Almost like a nightmare.
When you know youre dreaming and you just want to wake up and everything to be ok.
It sometimes hard to realise that its real life because youre hoping so much that it just a dream that you can wake up from.
Anxiety can target anything, things that would be considered scary by most people – and then some things that aren’t even normally scary suddenly start becoming daunting – and even you don’t know why, things like going shopping, talking to people, leaving the house, it all becomes such a worry.
It not like a little worry, it like a full blown fear.
People constantly telling you to face it and you just wishing it was that simple.
Having to accept that it going to hang over you and having to calm your brain down by cancelling what is worrying you.
People thinking that you’re just making a big fuss out of nothing when in reality they can’t even being to imagine the panic response is giving off.
Better yet talking about it seems impossible because even when people say they understand they still want you to do whatever is scaring you and something inside of you is stopping you and so you get angry, you’re so done with being sad or scared, you just feel anger, frustration and hurt, hurt because all you want is a hug and someone to reassure you but really they get mad.
Raise their voice. Get frustrated, Say ‘why can’t you just do it?’
because it’s hard that’s why.
It may seem easy for you but hey try living like me, when everything is scary, the only place I feel calm is my home and even the thought of leaving it almost scares me enough to bring me to tears, feeling sick, feeling horrible, and feeling like a disappointment, all because this stupid mental illness won’t leave me alone.
( Written by a 17 year old)

OCD (obsessive compulsive disorder) can be extremely disruptive and distressing for those that struggle with the disorder. Today on the blog, a member of the Mind team talks about their experience with OCD and how they have found ways to manage it.
If another person was doing this, you might call it abuse or bullying. Someone who says, over and over: “No. That’s not good enough. Do it again.” Who torments you and won’t let you go to sleep. You might even call it torture.
Except it’s happening inside my own head, so I can’t get away from it. That’s what obsessive compulsive disorder (OCD) feels like: it’s a bully I can’t escape from.
Some people think OCD is a joke, or it’s just being really neat or tidy. That’s not what it’s like.
Read more: https://www.mind.org.uk/information-support/your-stories/ocd-and-me/#.Whdw8Upl-M9
Struggling to work because of mental health?
If your work is being affected by depression, anxiety, stress or other mental health issues then we can help you. We offer a free and confidential Mental Health Support Service available to anyone with a mental health condition who is absent from work or finding work difficult. It is aimed at helping people to remain in, or return to, their role.
Chris, a high profile Assistant Director of Operations for a housing association suffered a nervous breakdown which meant that his work suffered. Working with Remploy meant that he was able to return to the workplace with his Employer being better informed and able to support him. Watch his video.
Read more at: http://www.remploy.co.uk/info/20137/partners_and_programmes/227/workplace_mental_health_support_service
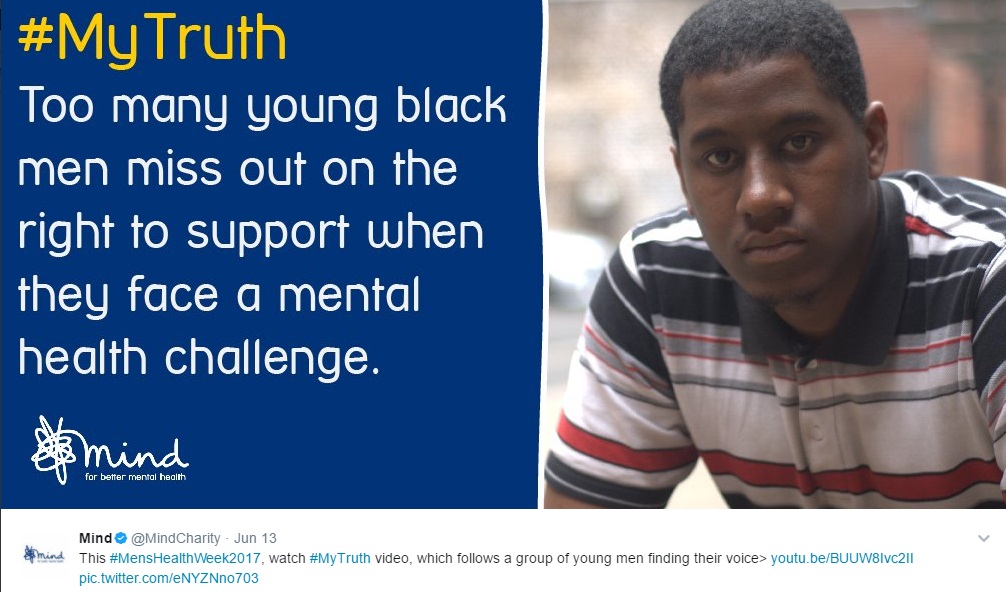
Four young men in a barbershop have to face their own truth. What’s your truth? Watch #mytruth now>
Helplines, coping strategies and Media
Mental Health in Manchester (MHIM) is a site for Manchester people who want to know more about how to look after their emotional health and wellbeing.
Have you seen these fantastic self-help guides?
5 Ways to Wellbeing January 2016
Distress to De-Stress January 2016
Visit the website for more information and support: http://www.mhim.org.uk/

Help us improve our information
If you’d like to get involved in improving Mind’s information, you can either become a reviewer, or submit a quote.
Become a Mind reviewer

To make sure all of our 100+ information resources reflect real life and are genuinely helpful for people, each one is reviewed by people with personal or professional experience of the topic before they are published.
Could you help us by being one of them?
Reviewers who are selected and who complete the review before the agreed deadline will be paid £25.
Manchester Suicide Prevention Partnership
In Manchester, a suicide prevention partnership has been formed to tackle and progress the suicide prevention agenda at a local level. It has agreed that:
- We all have a role to play in prevention, it is everyone’s business
- One suicide is too many
- Suicidal thoughts are common, this is perfectly normal
- Building strong, resilient communities is a powerful antidote to suicide
- Talking about suicide actively tackles stigma
- There is help available in Manchester
Help In Manchester
If you or someone you are caring for needs help then you can contact your GP for an emergency appointment or visit you local Accident and Emergency Department.
A guide to tackling suicidal thoughts is available here.
For non urgent support in Manchester visit the Mental Health in Manchester (MHIM) website for further details of services in the city.
Helplines:
- Samaritans: 116 123
- Saneline: 0300 304 7000
Welcome to Manchester Mind
Please note that our main number has now changed to 0161 769 5732.
Manchester Mind is in independent local mental health charity which delivers services to young people and adults. Our vision is of a city that promotes good mental health and treats people with mental health problems positively, fairly and with respect.
We are committed to improving the lives of people with mental health needs. We promote the health and wellbeing of people affected by mental distress and take a positive approach to mental health, challenging stereotypes and discrimination.
We listen to and respect people who use our services, value their experiences and place them at the centre of service delivery and development. We enable people with mental health needs to improve their health and wellbeing to reach their full potential. We work with people so they can live more successfully in their communities. Above all, we aim to create a positive future for people who use our services or volunteer.
Read more at: http://www.manchestermind.org/index.php
Moodswings is an award winning Manchester based Charity founded in 1999 to help people recover from mood problems and the severe emotional distress they can cause.
Mood problems can range from periods of severe anxiety or depression to episodes of high and low mood. The effects on education, employment, relationships and family life can be devastating.
The work of the Charity is based on a belief that people can recover from severe mood problems and move on to lead happier and fuller lives.
From its centre in Manchester, Moodswings reaches out across the north west and beyond with a message of real hope and optimism for individuals and their families and friends.
Our evidence-based, down to earth approach is reflected in the range of innovative services we provide.
Read more at: http://www.moodswings.org.uk/

Buzz Health & Wellbeing Service for people and communities in Manchester.

free online support for young people
Get real time help with friendly, qualified counsellors.
Free. Safe. Anonymous.
https://www.kooth.com/index.php
 The Horsfall is an exciting new venue and programme of activity building on 42nd Street trusted and innovative approach to improving young people mental health.
The Horsfall is an exciting new venue and programme of activity building on 42nd Street trusted and innovative approach to improving young people mental health.

Please note that our main number has now changed to 0161 769 5732.
CALM helpline now open 5pm – midnight. Anonymous and confidential support for men. 0800 585858.

This is an idea we developed for testing.
Depression and anxiety
- How to tell if you have depression or anxiety
- Seeking help
How to tell if you have depression or anxiety
Everyone has periods of low mood. Sometimes this can be because of a particular event, eg a break up.
Usually low mood gets better on its own after a short time. If it doesnt, this could be a sign of depression or anxiety.
Symptoms of depression
When youre depressed you often have the symptoms for weeks. They can be so bad that they start to affect your daily life, eg your work, your family and social life.
The symptoms of depression can be complex but they often include the following:
- feeling low and sad all the time
- feeling hopeless and helpless
- feeling anxious and worried
- low self-esteem
- feeling tearful
- being easily irritated by others
It can affect your body, too:
- problems getting to sleep or sleeping too much
- not feeling hungry or eating too much
- unexplained physical symptoms, eg aches and pains
- lack of energy
- no interest in sex
- headaches that keep coming back or dont go away
Symptoms of anxiety
If you feel anxious all the time and the feeling isnt about one specific thing you might have generalised anxiety disorder.
Symptoms of anxiety include:
- feeling restless
- worrying that things go wrong
- being on edge a lot
- not concentrating
- feeling irritated by things
- avoiding going out or seeing people
Your body can also change and you might notice these symptoms:
- feeling dizzy
- problems sleeping or constant tiredness
- stronger and irregular heartbeat
- trembling or shaking
- headache
- stomach ache or feeling sick
What to do next
If you think you have any of the symptoms for depression and anxiety, you should seek help as soon as possible.
http://nhsalpha.herokuapp.com/depression-and-anxiety/how-to-tell-if-you-have-depression-or-anxiety

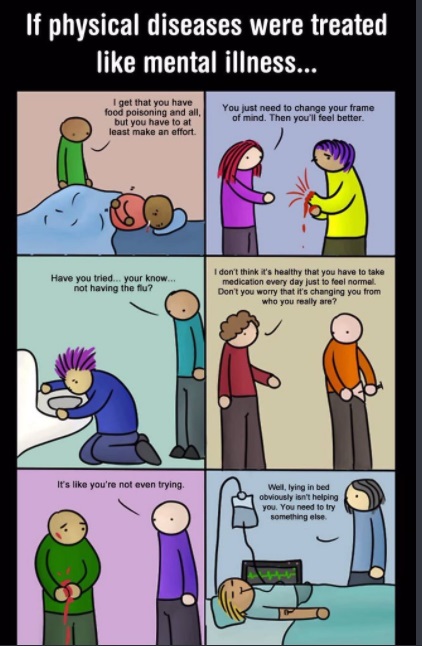
Serious illness can be a tricky thing to explain to children at the best of times. While it relatively easy for them to understand physical pain or injury, how do you explain mental illness to children?
At the end of 2013 my husband was diagnosed with bipolar disorder and severe anxiety. Wed been together for more than eleven years and had two children: a daughter then aged four and a half, and a son who was about to turn two. The diagnosis was a surprise to both of us; although hed had occasional periods of depression, he was generally a happy and enthusiastic man who took care of me when my own mental health wasnt great. (I have cyclothymia and suffered with severe post-natal depression after the births of both children; thanks to medication and an outstanding GP Im well these days).
It soon became clear that not only was the diagnosis correct but that it was long overdue. What my husband and I had innocently thought were long periods of normality interspersed with depression turned out to be periods of hypomania interspersed with depression. It was all so obvious once we knew what to look for.
Bipolar disorder can be hard to live with, both for the person with it and their family. Previously known as manic depression it causes the individual mood to swing unpredictably between highs and lows. The highs are known as mania and are often characterised by very energetic behaviour, enthusiasm, and sometimes impatience.
The lows of course are depression and cause feelings of sadness, worthlessness, worry and extreme tiredness. While medication and psychiatric support can lessen the effects (so the highs are less high, the lows arent so low and hopefully the periods in between are longer!) it still a difficult illness to live with. The anxiety doesnt help; my husband often feels uncomfortable in crowds or social situations, and rarely leaves the flat without me.
Dont get me wrong – my husband is a kind, loving man and a fantastic father. But mental illness isnt something that easy to talk about in our society. There a stigma attached to it that simply isnt there where physical ailments are concerned, and this can isolate not just the person with the illness but also their family. My husband and I used to be very open about our health issues; until, that is, a friend who hadnt seen us since before the children were born reported us to the NSPCC as unfit parents, solely because we both have a mental health diagnosis. Naturally Children Services investigated and cleared us fully, but for a long time we felt unable to talk to anyone outside the NHS or our immediate family.
Now that our children are older (theyre 6 and 3.5) theyre more aware that their dad isnt like other dads and have begun asking questions. Why is Daddy sad? Why is Daddy still asleep? Why does Daddy have so many headaches? Weve discussed these and many more questions several times now, and Id like to share several key things to remember when explaining mental illness to children.
First of all, keep it simple and age-appropriate. This may seem obvious but it surprisingly difficult! When talking to our six year old weve explained that part of Daddy brain doesnt work properly, and so sometimes he gets sad or cross even if he doesnt want to be. Our three year old understands that sometimes Daddy has sad days when he sleeps a lot. They both understand that Daddy takes special medicine to help his brain work better.
Be honest. You dont have to be explicit or even detailed about the illness and its effects, but do tell the truth (again, in an age-appropriate way). Children are very good at detecting when an adult is covering something up, and they need to know that you will be open and honest with them.
Reassure them that the illness isnt their fault. For young children especially, the world revolves around them and the way that adults behave is, in their mind, directly related to their behaviour and feelings. Explain that they are not responsible for how the person with the illness feels or behaves.
Make sure that the child understands that it not their job to look after the ill person either. There a very fine line between a child being aware and understanding of an adult illness, and trying to protect and care for them. Ive made it very clear to our children that looking after Daddy is my job, not theirs. That not to say that they cant be considerate (no bouncing on Daddy when he having a sad day!) but you need to be firm that their only job is to be a child.
Can Daddy brain be fixed? This is the question I find the hardest to answer. Sometimes mental illness is curable and sometimes it merely manageable; bipolar disorder falls into the latter category. Again, be honest: if it possible that the person will recover, say so but explain that it may take time. If the illness is only manageable, explain that too but try to emphasise that that ok.
Let the child know that youre always there for them to talk to and that they can always ask questions. If the person with the illness agrees, remind the child they they can talk to them as well. As the child gets older they will think of more questions and be able to understand more, so be prepared to have conversations about mental illness every now and again.
If your child attends school, consider making their teacher or keyworker aware of their relationship with the ill person. When my husband has a prolonged period of depression our daughter feels it keenly, and if she should become upset or behave out of character at school it reassuring to know that an adult there will understand why and be able to help her.
Above all, be calm, honest and reassuring, and then carry on as normal.


Welcome to Students Against Depression
Are you or someone you care about feeling persistently sad, low, anxious or empty? Depression is more common than you might think – 1 in 10 people will experience depression and/or anxiety in any one year.
Students Against Depression offers information and resources validated by health professionals alongside tips and advice from students who have experienced it all themselves.
You are not alone and we are here for you. Download our resources, customise our self help plans, share your own story and join us in fighting student depression.
Students Against Depression offers comprehensive, award-winning information and resources to help you identify low mood or depression and then find a way forward.
Visit the website to find out more: http://studentsagainstdepression.org/
Returning to work after mental health issues
If you’ve had time away from work, or have been long-term unemployed because of mental or emotional health problems, you’re not alone. Almost 50% of long-term absences from work are the result of mental health issues, including depression, anxiety and bipolar disorder.
People who have had a mental health problem and been out of work often worry about going back. Common concerns include facing discrimination or bullying, and going back too soon and feeling unwell again.
According to a report by the Royal College of Psychiatrists on mental health and work, “Many people with mental health problems fear that, no matter how good a recovery they have made, their symptoms will be made worse by going back to work.”
How work benefits mental health
Although work can cause stress for some people in some situations, recent research shows that for most people:
- work is beneficial to health and wellbeing
- not being in work is detrimental to health and wellbeing
- re-employment after a period of being out of work leads to an improvement in health and wellbeing
The benefits of being in work can include:
- a greater sense of identity and purpose
- an opportunity to build new friendships
- an improved financial situation and security
- a feeling that you’re playing an active part in society
Get the free Mental Health & Debt guide

This is a free 44-page PDF booklet supported by Mind, Rethink, CAPUK and others, for people with mental health problems and those caring for them.
It covers how to handle debts when unwell, work with banks, free debt counselling, specific tips for bipolar disorder or depression sufferers, whether to declare a condition and more.
http://www.moneysavingexpert.com/credit-cards/mental-health-guide

Chorlton Anxiety Group
This drop-in group offers a sympathetic and non-judgmental space where you can meet others who also struggle with anxiety. Our groups care about your experiences and really understand. They offer help, information and a place for people to share ideas on how to cope with anxiety.
- Opening times:
- Every Tuesday from 7.00pm – 9.00pm
- Access:
- If you haven’t attend the group before, give us a call or send us an email to let us know you are coming, and we will make sure someone is there to greet you.
- Age:
- 16+
- Cost:
- Free
- Related:
- Anxiety Anxious Depression Emotional Feeling Down Group Hopeless Low Mood Peer Sad Stress Support Tearful Unhappy Worried Worry
Urgent Help
IN AN EMERGENCY:
– Contact your General Practitioner (GP)
– Call your nearest NHS Walk-In Centre or go to Accident & Emergency (A&E) at your local hospital. Click here to find your nearest walk-in centre online
YOU CAN ALSO CONTACT THESE ORGANISATIONS FOR SUPPORT
Mind Infoline Deaf people can access this service by dialing 18001 before the telephone number. Monday to Friday: 9.15am to 5.15pm. 0845 766 0163 | info@mind.org.uk | Click here to visit the Mind website.
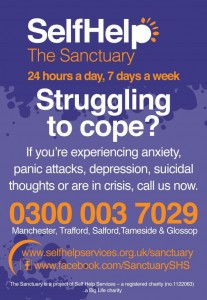
The Sanctuary Overnight, every night service providing a place of safety and support to adults feeling at crisis point and living with difficulties such as panic attacks, depression and low mood. 8pm-6am. 0161 637 0808 | Click here to visit their website.
Crisis Point Helping people with diverse needs to resolve their current crisis and develop strategies to prevent or better manage future crises. Open-access mental health crisis centre. Bespoke crisis management support. 0161 225 9500 | Click here to visit their website.
Rethink Deaf people can access this service by dialing 18001 before the telephone number. Monday, Wednesday, Friday: 10am to 3pm | Tuesday & Thursday: 10am to 1pm. 020 8974 6814 | advice@rethink.org
SANEline For anyone affected by mental illness (service users, their families, carers, health professionals). Deaf people can access this service by dialing 18001 before the telephone number. Mon-Fri: 12noon to 11pm | Sat-Sun: 12noon to 6pm 0845 767 8000
Samaritans 24-hour confidential emotional support. 08457 90 90 90 | jo@samaritans.org

Introduction: the scale of the challenge
THE MANIFESTO
- Face up to reality
- Invest in research
- Focus on prevention – no let-up on big killers
- Dont wait for men to engage – especially on mental health
- Design targeted programmes around the needs and attitudes of the highest risk men & boys
- Tailored health awareness and literacy, especially amongst boys
- Organisational focus across the whole health system
OUR CHALLENGES
- Our Challenges to NHS England
- Our Challenges to GPs
- Our Challenges to Public Health England
- Our Challenges to Local health systems
- Our Challenges to Men
References
Download a PDF of the manifesto (PDF, 263kb)
Sign up to support the Manifesto
DON’T WAIT FOR MEN TO ENGAGE – ESPECIALLY ON MENTAL HEALTH
Remove the barriers to using health care, mental health and preventative care – especially for men of working age:
- Sort out opening times and access so they work for full-time workers
- Improve online access, booking and other interaction
- Stop using drug or alcohol problems as a barrier to mental health treatment – invest in integrated care for dual diagnosis
- Deliver on the recently announced access & waiting time standards for mental health
- Tackle stigma and discrimination, especially in the workplace and especially for men with stigmatised problems such as mental health, eating disorders, breast cancer and sexual violation
- Greater use of self-help groups and peer-led services.
Reach out proactively:
- Take services to where men are: workplaces, online, pubs, sports grounds, betting shops, prisons etc.
- Where it not already happening, extend occupational health to include screening and preventative health measures
- Create a Mental Health Diversion Duty in the criminal justice system and emergency care – intervening more effectively to reduce the number of people arrested under Section 136. Deliver national coverage by 2017
- Increase health check outreach and uptake amongst men
- Start bowel cancer screening earlier, especially for higher risk men, including MSM.
Make the most of it when men do engage with health services:
- Include cancer symptom awareness, mental health, sleep apnoea and erectile dysfunction in health checks
- Special focus on high-risk infrequent attenders
- Co-design new services with men.
WHY IS THIS IMPORTANT?
Health services are still not effectively engaging with men. Especially during working age, men remain less likely to:
- attend a general practitioner
- attend a NHS Health Check
- opt for bowel cancer screening
- visit a pharmacy
- take a Chlamydia test
- have a dental check-up.
Four in five suicides are male but only a minority of these men were engaged with mental health services.
67% of men are overweight or obese yet only 10-20% of those on NHS weightloss programmes are men.
Research has suggested a link between men lower use of primary care and their higher rate of hospital services.
71% of CVD-related deaths under 65 are amongst men14 and the NHS Health Check programme focuses on circulatory conditions, a major killer of men, yet only 35% of local authorities know how many men they reach with the
programme,15 and within those authorities only 44% of health checks are conducted amongst men.
Community Services
Community Services are the foundation of Self Help providing community based self help initiatives.
Drop-in Groups
These Drop-in Groups are available for anyone living with conditions related to each group.
Unless otherwise stated our Drop-in Groups are funded by Manchester CCG
ZION ANXIETY GROUP
This group runs every Wednesday 1-3pm.
Venue: Zion Centre, 339 Stretford Rd, Hulme, Manchester M15 4ZY.
ZION DEPRESSION GROUP
This group runs every Wednesday 3-5pm. Venue: Zion Centre, 339 Stretford Rd, Hulme, Manchester M15 4ZY
CHORLTON ANXIETY GROUP
This group runs every Tuesday 7-9pm
Venue: Chorlton Methodist Church, Manchester Road, Chorlton, Manchester M21 9JG.
MANCHESTER SOCIAL PHOBIA GROUP
This group runs every Tuesday 7-9pm.
Venue: Kath Locke Centre, 123 Moss Lane West, Moss Side, Manchester M15 5DD.
HARPURHEY DEPRESSION GROUP
This group runs every Thursday 1-3pm.
Venue: North City Library, Rochdale Road, Harpurhey, Manchester M9 4AF.
WYTHENSHAWE ANXIETY GROUP
This group runs every Saturday 10am-12pm .
Venue: Macmillan Room, Wythenshawe Forum Library, Forum Square, Wythenshawe, Manchester M22 5RX.
Please contact the Community Services Team for more details: communityservices@selfhelpservices.org.uk or 0161 226 3871.
URMSTON DEPRESSION GROUP
This group runs every Tuesday 1.30-3.30pm.
Venue: Urmston Library, Unit 34, Golden Way, Urmston, Manchester M41 0NA.
This service is currently funded by Trafford CCG.
ALTRINCHAM ANXIETY GROUP
This group runs every Monday 1-3pm.
Venue: St George Parish Church, Church Way, Altrincham WA14 4DW
This service is currently funded by Trafford CCG.
OPENSHAW WELLBEING GROUP
This group is held on alternate Fridays 1-3pm.
Venue: The New Roundhouse, 1328 Ashton Old Road, Openshaw, Manchester M11 1JG.
This group is funded by Manchester Settlement.
Courses
BOOST: EMOTIONAL RESILIENCE COURSE
The BOOST: Emotional Resilience Course is a 6-week structured course which helps people to cope better with life ups and downs and respond to challenging situations positively. The course is aimed at individuals who are experiencing a range of life issues such as anxiety or low mood, loss, relationships issues, work stress and carer responsibilities. The course gives participants the opportunity to meet and talk together in a mutually supportive atmosphere and build strategies to improve their resilience, confidence and general wellbeing.
Please see our website for updated course times and venues or contact the Community Services Team atcommunityservices@selfhelpservices.org.uk or 0161 226 3871 for more details.
Personality Disorder Project
Personality Disorder Multi-Agency Development Service
Funded by Salford NHS CCG to raise awareness of Personality Disorder this projects aims to create a multi-agency network by holding regular forum meetings to discuss and highlight gaps in this field, to share good practice and work together to improve the experience of people suffering from Personality Disorder accessing services in Salford.
The project also works with agencies across Salford by delivering awareness training. If you work in Salford, or with clients who live in Salford, then you can access the Personality Disorder Awareness training.
For more information on the training provided by this project or when the next training sessions are please contactnina.bradshaw@selfhelpservices.org.uk
Peer to Peer Service
Our new Peer to Peer service provides an innovative new dimension to our Community Services provision. Building on the success of our After Therapy service, the Peer to Peer service promotes the culture and practice of Peer experts who have gained experience of mental health difficulties and the steps that are necessary to create a successful recovery, through direct first hand experience.
Referral information
The Peer to Peer service is suitable for individuals who are experiencing common mental health problems such as anxiety and depression. It can also be useful for the following situations:
– People who are dont engage well with more clinical types of mental health services.
– People who are considering accessing some sort of therapeutic or wellbeing help and want support and guidance around the range of options to help improve their mental health.
– People who are leaving therapy and want some “after therapy†support to continue the recovery work that they have started.
– People who are currently accessing therapeutic intervention and need more support to build their recovery package.
This service is not suitable for people presenting with a high level of risk.
Our service might also be unsuitable for individuals presenting with more severe and enduring / complex conditions of mental distress. A general guideline that we ask referrers to consider is “is this person likely to achieve change/improvement by working towards wellbeing goals with a volunteer peer mentor over a period of six monthsâ€.
Home Connect
Home Connect is designed for people who are new to Self Help and who are making initial enquiries into our services on the phone. Peer to Peer volunteers (in pairs) can arrange to visit an individual at home, or at a nearby community location to discuss what services we have to help them and what other support is available in the local community. They can help individuals where appropriate to complete referral forms and can accompany people to first appointments or engagements with drop in groups and other services.
Peer to Peer Mentors
For up to six months, regular sessions through meetings or phone support can be arranged with our Peer Mentors, experts by experience in wellbeing and recovery, for individuals experiencing a range of mental health difficulties. This service provides a real bridge to healthy interdependent wellbeing based on real firsthand experience of what has worked in the lives of fellow recovering peers.
Location: Peer Mentoring is available at a variety of venues in Manchester, Salford and Trafford. Please note that we unfortunately do not cover Stockport, Oldham, Bolton or any areas outside of Greater Manchester.
Recovery Workshops
Our team of Peer to Peer experts provide a comprehensive overview of the essential steps for a successful recovery from mental ill health. Taking a radical break from the clinical focus of traditional services and placing greater emphasis on shared learning, healthy community, experts by experience and the healing power of the peer relationship, these workshops help participants make the successful journey from stuck, to recovering, to thriving!
This service is available across Greater Manchester.
For more information on any of our Peer to Peer services please contact phil.girling@selfhelpservices.org.uk orkate.jolley@selfhelpservices.org.uk or telephone 0161 226 3871
The Peer to Peer service has been created with help from The Big Lottery Reaching Communities funding programme.
Welcome to Manchester Mind
Please note that our main number has now changed to 0161 769 5732.
Manchester Mind is in independent local mental health charity which delivers services to young people and adults. Our vision is of a city that promotes good mental health and treats people with mental health problems positively, fairly and with respect.
We are committed to improving the lives of people with mental health needs. We promote the health and wellbeing of people affected by mental distress and take a positive approach to mental health, challenging stereotypes and discrimination.
We listen to and respect people who use our services, value their experiences and place them at the centre of service delivery and development. We enable people with mental health needs to improve their health and wellbeing to reach their full potential. We work with people so they can live more successfully in their communities. Above all, we aim to create a positive future for people who use our services or volunteer. http://www.manchestermind.org/index.php

What is resilience?
Building a Healthy Future is a course devised to help people improve their mental health and to develop resilience. All of us will experience difficult times in our lives. How we respond to those has a big impact on our wellbeing. While we cant choose what happens to us, we can choose in how we respond to challenging, stressful or negative events. It not always easy, and may not come naturally, but we can learn to change our mindset. Research shows that resilience isn’t a rare quality found in a few, extraordinary people and that resilience – like other life skills – can be learned.
Read more:
https://www.whalleyrange.org/?p=3582
Mental wellbeing “a dynamic state in which the individual is able to develop their potential, work productively and creatively, build strong and positive relationships with others and contribute to their community. It is enhanced when an individual is able to fulfil their personal and social goals and achieve a sense of purpose in society†Or “Feeling good and functioning wellâ€
Community Counselling Service
We can offer the Counselling sessions from our office in Old Trafford, from the Individuals GP Surgery or a venue closer to their home.
We may provide Counselling within the Individuals home if they are housebound, however the sessions must be private, confidential and not disturbed by others.
If Individuals cannot speak English we will provide a Counsellor who speaks the same language or offer support via an Interpreter.
The Community Counselling Service sessions last approximately 50 minutes and are offered on a weekly basis. During the first session the Counsellor may perform an initial assessment of the Individual’s needs and determine the suitability of the service being offered. At this stage there may be an initial agreement of the number of sessions provided which is typically 6 (subject to review) or the Individual may be referred to another service. Once an agreement has been made to undertake Counselling, Individuals are expected to attend regularly to fully benefit from the service.
Community Counselling Service Referral Form
WRAP: This is an American website but contains loads of useful information: http://mentalhealthrecovery.com/wrap-is/
All about us!
So who are we?
Were a Manchester Catering social enterprise based in the Zion Community Resource Centre in Hulme and provide a whole range of catering options at competitive prices across Manchester. We became a social business in 2005 and since then have catered for events of all sizes and types across Manchester.
What is unique about our enterprise is that we are also part of a local mental health charity, Manchester Mind – who provides a wide range of services to support and empower people with mental health problems – through provision of advice, volunteering, mentoring, counselling (for young people).
All our services are about building resilience and enabling people to gain mental wellbeing. A significant number of our volunteers go back into work, education or further volunteering with reported improvements in their mental health. To find out more about the charities work www.manchestermind.org or click here to see our latest annual report.
Profits made by Good Mood Food are reinvested in to Manchester Mind to help more people with mental health problems to benefit from our wide range of services.
Read more: http://goodmoodfood.org/
Old Trafford Wellbeing Centre
Old Trafford Wellbeing Centre is a community wellbeing hub run by and for the benefit of local residents with support from blueSCI a not for profit social enterprise which supports people who may be experiencing emotional or psychological distress. The aim of the centre is to support local individuals and families to achieve their goals and improve their health and wellbeing through the 5 Ways to Wellbeing;
http://oldtraffordwellbeing.org.uk/about-us/
ACMHS is a voluntary/charitable organisation, which has been in existence for over 24 years.

The African and Caribbean Mental Health Services (ACMHS) is a community organisation based in Central Manchester providing free, confidential, sensitive and culturally appropriate services to African and African Caribbean people suffering from mental ill health.
The organisation was established in October 1989 and provides services across economic and socially disadvantaged areas within Manchester for people in hospitals or the community experiencing mild to moderate and enduring mental health conditions, for example, schizophrenia, bipolar disorders and common mental health issues.
Find out more: http://acmhs.squarespace.com/

Mind and body – stay healthy online from Learn My Way
Looking after your mental health
Health isnt just about the body – it important to look after your mind and your mental health too. Weve put together a new page on Learn My Way to help you do just that.
Whether you want to help yourself or a friend, our page has plenty of ways you can take positive steps. Join an online community, find someone you can talk to or watch videos from NHS Moodzone to support you on your way to feeling better.
Take a look at the new Mental Health page on Learn My Way: http://tinyurl.com/o7o2ds7
Relaxation for children
(http://www.moodcafe.co.uk/for-children-and-young-people/relaxation-for-children.aspx)
Relaxation Exercises for Children
Relaxation exercises help children to manage their reactions to stress, anxiety and worry. Relaxation exercises are a good distraction from worrying thoughts and reduce tension in the body. The exercises here include controlled breathing, muscle relaxation and guided imagery.
Controlled Breathing and Muscle Relaxation
Long, deep controlled breaths slow down the breathing rate and help children to relax. Muscle relaxation involves practicing tensing and relaxing different muscles in the body. This helps children to recognise the difference between tense and relaxed muscles.
Relax like a cat is a colourful leaflet for younger children to practice controlled breathing and muscle relaxation. It is best to sit down and read it with your child at a quiet time of day when there are no worries or stresses. Or, your child can listen to the audio version. There is a female voice and a male voice to suit your child’s preference.
Guided imagery
Children can close their eyes and listen to a voice guiding them through a soothing and calm imaginary scene. Children can also make up their own soothing image. For example, this could be a favourite place that makes them feel calm. Ask your child for details (e.g. what they can see, hear or smell) so you create the image together.
Practising
Practising relaxation exercises daily helps children learn how to relax and calm themselves. To begin with, it is best to practise when there is no distress. Encourage your child to practise at least once a day and when there is little chance of interruption or distraction. Once they have learned the exercises, they can be encouraged to use the techniques when they are feeling stressed or anxious.
Older children and teenagers will also benefit from doing regular relaxation.